Nutrition
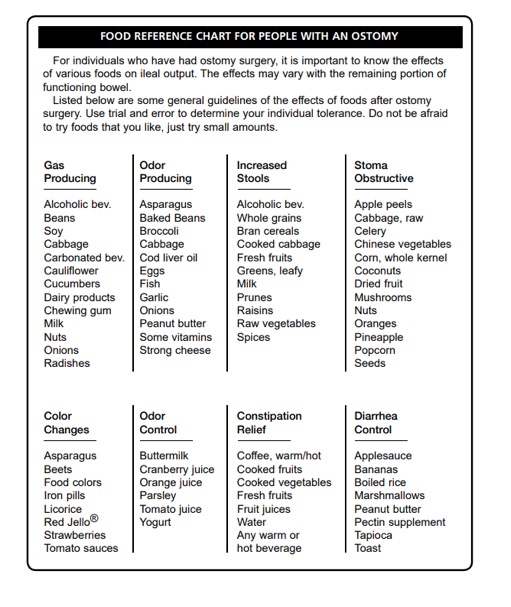
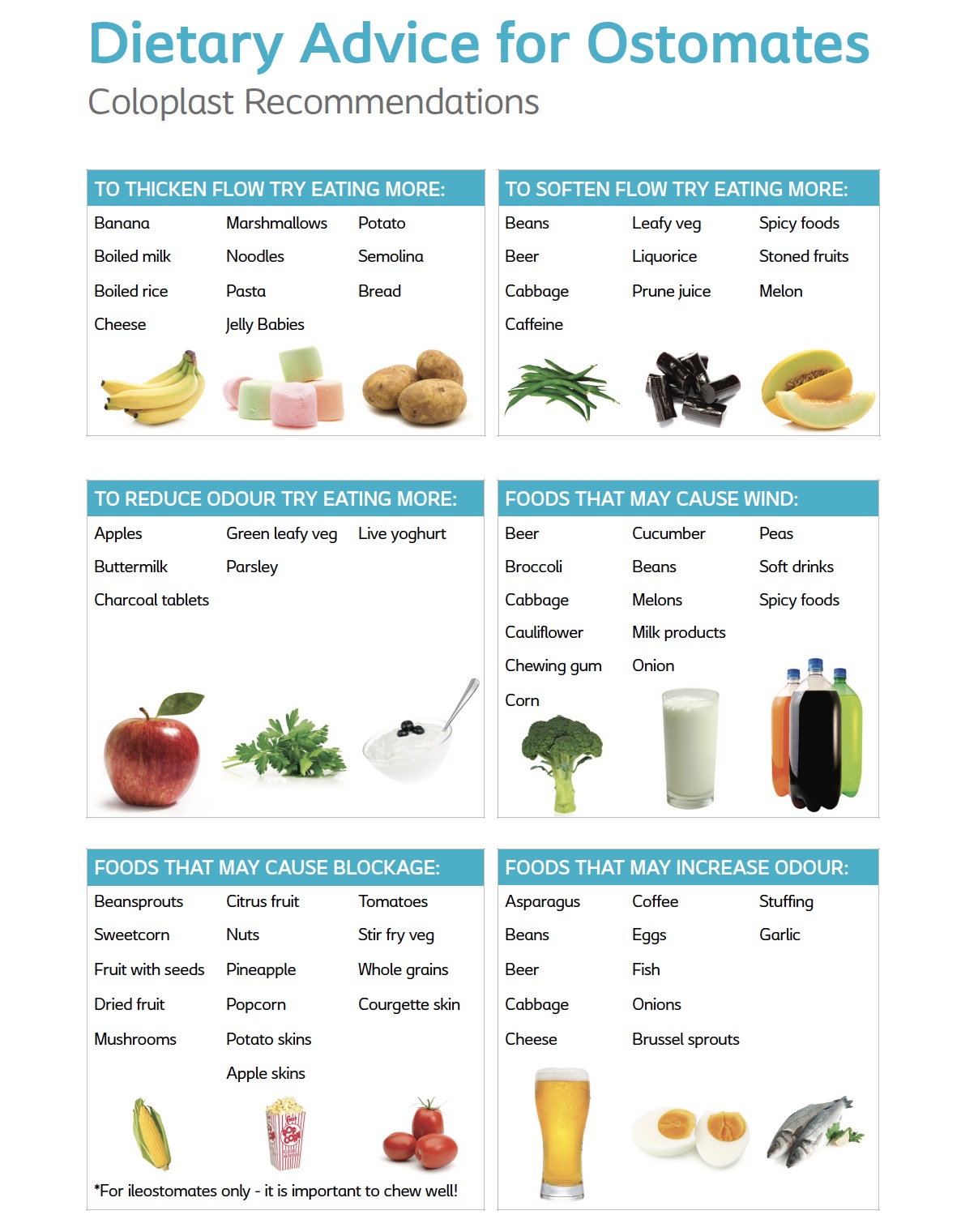
There is no specific “Ostomy Diet” but there are important considerations as you discover the foods that work best for you. For guidance always follow a GP or Stoma Nurses orders at each stage of your post op adjustment. Individual sensitivity to certain foods varies greatly. You must determine, by trial, what is best for you. A guide as below can help in this process.
Your appetite should gradually return after ostomy surgery
Initially after your operation, you might find that your appetite is smaller than normal and that you feel like you’re bloated or have indigestion after meals. However, as you become more active, you should find that your appetite returns and that you don’t experience these symptoms anymore. If you feel that you can’t face a full meal, soups and milky drinks are a nourishing alternative.
Aiming for regular bowel movements
As you get better, these practical tips will help you to have regular bowel movements (both in frequency and consistency):
- Don’t under eat – have 3 regular meals a day. You may experience irregular bowel movements and excessive wind if you don’t eat regularly
- Try to eat a balanced diet with low fat and moderate fibre intake. You shouldn’t cut out high fibre foods entirely as these contain lots of vitamins and minerals necessary to our diet
- Drink plenty of fluids – aim to drink around 8-10 large mugs of fluid a day e.g. water, squash, tea, coffee or milk, unless you have been advised not to (for example, if you have a particularly high output ileostomy)
- Take gentle exercise
It’s not just an ‘Old Wives’ Tale: chew your food well if you want to avoid excess wind and have more consistent bowel movements!
You might find that certain foods cause your output to change consistency to begin with after your surgery. Rather than ‘banning’ them immediately, it’s worth experimenting with these foods a few times before excluding them from your diet – you might well find that you can eat them again in a few months’ time, once your body has adjusted to the new situation.
Always follow the guidelines of your GP, Stoma Nurse and your own body as each ostomate is different and we all process our food differently. You will find your own way through experimenting with food.
Special Considerations
Blockages and dehydration – Those that have had ileostomy surgery are most at risk of blockages and dehydration but good practice for all is to hydrate properly and thoroughly chew your food. If you suspect a blockage it requires quick attention and often an emergency visit to the GP or hospital.
Nutrition Support is most commonly used for Vitamin B12 absorption issues. In other severe cases intravenous and tube feeding may be needed.
Short Bowel Syndrome (SBS, Short Gut) is a rare but sever malabsorption issue. Short bowel syndrome generally occurs when a large portion of the small intestine has been removed by surgery or as a result of disease or injury. Know the symptoms and talk to a doctor to see if you are at risk.
Gas/Wind/Flatus
Some people produce more wind than others. If you experienced problems with wind before the surgery this will not change after surgery.
Wind can result from swallowing air and after drinking fizzy/gassy drinks, talking when eating, smoking, chewing gums and some foods.
Foods that may cause wind are (Add these foods to your diet gradually and see how they suit you.)
- Cauliflower, broccoli, winter root crop vegetables
- Onions, garlic
- Apricot, bananas
- Cabbage, spinach
- Cucumbers
- Mushrooms
- Eggs
- Beer
- Lactose/wheat intolerance
- Pretzels
- Hints and tips to avoid wind:
- Charcoal tablets to be chewed
- Peppermint oil in hot water to drink
- Peppermint tea
- Cinnamon, to eat or drink (not if you are pregnant)
- Fennel, to eat or drink
- Angelica
- Sage, to eat or drink
- Yoghurt or yoghurt drinks

